Human Papillomavirus and Immune Health: A Hidden Epidemic
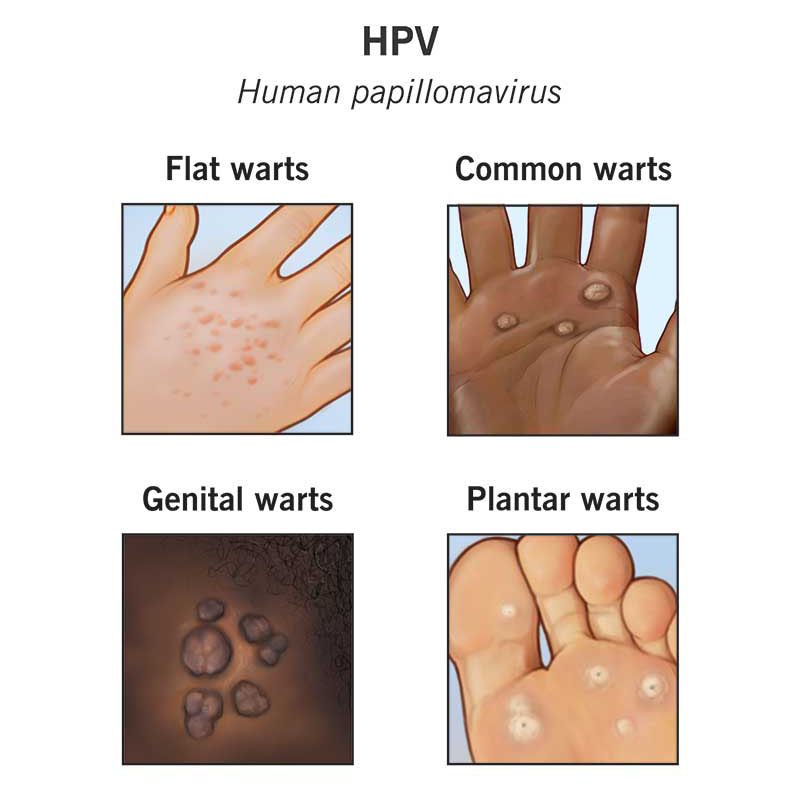
Human papillomavirus (HPV) is one of the most widespread infections across global populations. However, its systemic manifestations - most notably skin lesions, occur primarily in individuals with compromised immune systems. Virtually everyone encounters HPV at some point in their lives. In childhood, it often presents as warts on the fingers; in adulthood, these lesions can appear across various parts of the body. While such occurrences in children are natural, as the immune system is still developing, their presence in adults signals that the immune system may be failing to handle viral challenges effectively.
Debunking Myths About HPV
A common misconception is that HPV is untreatable and that nothing can be done to combat its effects. However, the immune system is equipped with mechanisms, such as natural killer (NK) cells, that can tackle viruses even without prior exposure or the production of antibodies. When numerous papillomas persist on the body, it often means these mechanisms are not functioning optimally. While millions live with this condition and it is normalized in many contexts, choosing to accept this as "just the way it is" doesn’t have to be your narrative.
Red Flags of a Weakened Immune System
Several key markers indicate poor immune function, many of which I’ve discussed previously. These include:
- Elevated ESR (erythrocyte sedimentation rate): Over 4 mm/hr in some cases.
- Imbalances in immune cells: High levels of neutrophils, eosinophils, or atypical lymphocytes.
- Digestive issues: Indicators such as undigested food in stool analyses.
- Metabolic dysfunctions: Insulin resistance, lipid profile abnormalities, and elevated homocysteine levels.
- Anemia: Low hemoglobin or iron levels can point to broader immune challenges.
Such markers are more than isolated findings - they collectively signal that your body may not be prepared to fend off viral threats. Recurrent colds, frequent infections, and visible HPV manifestations are all symptomatic of this vulnerability.
HPV as an Immune Litmus Test
Unlike many viral infections, the severity of HPV is uniquely visible. Simply counting the number of papillomas on your body can give a direct visual indication of immune health. A similar principle applies to herpes simplex virus (HSV), another common infection. Cold sores, for example, are not merely cosmetic nuisances - they’re outward signs of a severely weakened immune system.
Challenging "Normal" Perceptions
The normalization of these conditions by some healthcare professionals is deeply concerning. Accepting recurrent herpes outbreaks or widespread HPV manifestations as "normal" is a disservice to patient care. Instead, a proactive approach to bolstering immune health is crucial.
The Path to Immune Resilience
Improving immune function requires a multifaceted approach:
- Addressing Inflammation: Regularly monitor ESR, CRP, and immune cell counts.
- Optimizing Metabolic Health: Focus on reversing insulin resistance and correcting lipid imbalances.
- Strengthening Gut Health: Incorporate dietary changes to promote digestion and nutrient absorption.
- Combating Stressors: Minimize environmental toxins, adopt regular exercise, and prioritize restorative sleep.
For further exploration of how environmental and lifestyle factors impact immunity, consider The Autoimmune Solution by Dr. Amy Myers, which offers strategies to repair and strengthen the immune system. Similarly, Why We Get Sick by Dr. Benjamin Bikman provides insights into the links between insulin resistance and broader health issues.
Take Control of Your Health
You don’t have to live with visible signs of immune dysfunction. By actively working to enhance your immune resilience, you can not only combat HPV and herpes but also protect yourself from a host of other infections. Reject the normalization of poor immune health and strive for a standard of well-being that empowers you to thrive.
According to the materials: BIO-H.COM
